The spreading confusion: Rethinking Alzheimer’s disease
by Danielle Heller
Proteins are molecular machines. They perform an incredible diversity of tasks that enable all living cells to function. Like any machine, a protein must be properly assembled in order to carry out its specific task, and if something goes awry, the cellular consequences can be dire. Take Alzheimer’s disease for example. Alzheimer’s disease is the most common neurodegenerative disorder, affecting over 5 million people in the United States alone [1]. Alzheimer’s is a progressive disorder that manifests clinically as a loss of memory, personality traits, and the ability to carry out daily tasks [1]. Scientists do not fully understand why or how this disease develops, but it is known that in the brains of Alzheimer’s patients, some of these protein machines malfunction, forming large, toxic clumps. A major goal of Alzheimer’s research has been to uncover the causes and understand the consequences of this protein clumping. A recent study published in the journal Nature draws an interesting parallel between Alzheimer’s and prion diseases (e.g. “mad cow disease”), another group of neurodegenerative diseases caused by protein clumping. Prion diseases are unique for one important reason: they are infectious. This new study raises the important question: could Alzheimer’s too be infectious?
Proteins, amyloid, and prions, oh my!
A protein is made in a cell as a long, linear chain of building blocks, and interactions between these building blocks cause this chain to spontaneously fold into a specific three-dimensional (3D) shape. (For a more detailed explanation of protein folding, see reference 2). The correct folding of a protein into this 3D shape is essential for its proper function. In some instances, proteins can misfold and clump together to form aggregates, which can be very toxic to normal, healthy cells. The clumping of specific proteins is associated with a variety of disorders, notably Alzheimer’s disease and fatal prion diseases, which include the livestock disorder bovine spongiform encephalopathy (BSE) (commonly known as “mad cow disease”), as well as the human diseases, Kuru and Creutzfeldt-Jakob disease.
The two proteins that form protein aggregates in the brains of Alzheimer’s patients are amyloid-beta, referred to as Aβ, and tau. These Aβ and tau aggregates are thought to interfere with normal brain processes [3]. Prion diseases are caused by the toxic misfolding and clumping of the prion protein, PrP. Although Alzheimer’s is not a prion disease, and the PrP, Aβ, and tau proteins each normally fold into distinct 3D shapes, upon misfolding, all three proteins can all form aggregates that have a very specific structural pattern. When protein aggregates clump together in this specific pattern it is called “amyloid.” This structural pattern makes these amyloid aggregates highly stable compared to normal proteins; they are resistant to chemicals and degrading enzymes that typically destroy folded proteins or less structured aggregates. This means that once amyloid forms inside of brain cells it is not easy to get rid of.
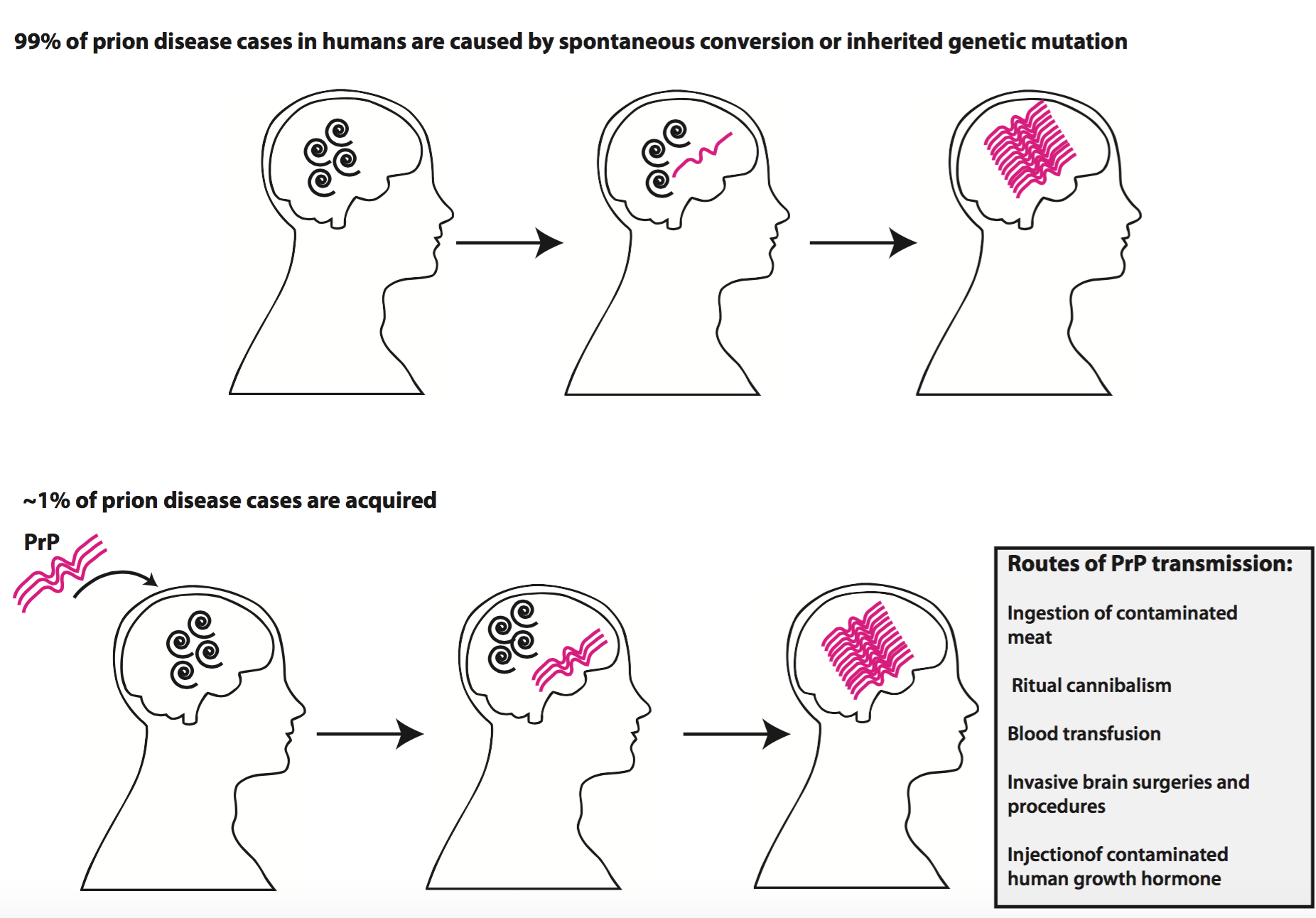
The protein-misfolding event that initially triggers the formation of amyloid aggregates in Alzheimer’s disease and in prion diseases is usually a spontaneous occurrence. It is known, however, that people can have certain inherited genetic mutations that can increase the likelihood of having these Aβ or PrP protein clumps form [3,4, 5]. Prion diseases, however, are remarkable in that they are infectious and can be transmitted from one person (or animal) to another [4,5].
Prions: a corrupting infection
Typically, when we think of infectious disease, we imagine a living microbe, such as a bacterium, invading our bodies, wreaking havoc, reproducing, and moving on to another host. A prion, however, is an infectious agent composed solely of misfolded PrP clumps that are able to corrupt properly folded PrP proteins within our cells. This infectivity of a PrP prion aggregate is a consequence of its ability to “self-propagate”[4,5]. As shown in Figure 1, within a brain’s pool of normally folded, functional PrP proteins, some molecules may spontaneously misfold into their prion form. These misfolded PrP molecules then act as templates that trigger the misfolding of other normal PrP molecules that they encounter. Such misfolding leads to a domino effect, as more and more proteins become misfolded and are incorporated into a large, growing amyloid assembly. If another individual’s pool of normal PrP is exposed to one of these templates, either through ingestion of contaminated meat or exposure to contaminated brain surgery tools, their PrP will also aggregate (Figure 2).

This unique (albeit very rare) infectivity of PrP aggregates has been the main reason that prion diseases and Alzheimer’s disease have traditionally been thought of as distinct disorders, despite their shared amyloid clumps. It has been known for several decades that PrP and Aβ behave similarly in a test tube, forming large amyloid assemblies. Only recently, however, have researchers been able to show that the amyloid aggregates involved in Alzheimer’s disease also have this self-propagating ability within brains [4,5]. In one study, mouse brain material containing Aβ aggregates was injected into a healthy mouse, triggering the formation of Aβ aggregates throughout its brain [5]. This and similar studies suggest that Alzheimer’s amyloid aggregates may have the potential to be infectious, similar to PrP aggregates. Thus, the only major remaining difference between prion aggregates and Alzheimer’s aggregates has been the lack of evidence that Alzheimer’s aggregates can be transmitted from human to human. New findings may bridge that last divide.
Evidence for human-to-human transmission of Aβ aggregates
Between 1958 and 1985, several thousand people mostly in the United Kingdom, France, and the United States were treated for short stature with injections of human growth hormone extracted from the brains of cadavers. This treatment was discontinued in 1985 after some patients were found to have acquired the human prion disease, Creutzfeldt-Jakob disease, from injected material contaminated with infectious PrP aggregates [6]. The cadavers from where the contaminated growth hormone had been extracted must have had undetected PrP aggregates within their brains. In a recent study published in the journal Nature, researchers from University College London performed autopsies on 8 individuals, all between the ages of 36 and 51, who had died from this acquired prion disease [6,7,8]. The researchers found PrP aggregates in the brains of all 8 patients, as expected; however, they were surprised to also find extensive Aβ clumps within the brains of 4 of the patients, and mild Aβ clumping in 3 more patients. Although none of these patients had been diagnosed with Alzheimer’s disease, it is extremely rare to find this type of Aβ aggregation in this age group, especially considering that the researchers found that none of these patients had any genetic mutations known to increase the likelihood of early onset Alzheimer’s. This finding caused the researchers to wonder: Could these Aβ aggregates also have been transmitted from the brains of the cadavers?
To confidently answer that question, the researchers needed to test a couple of hypotheses. First, does having PrP clumps make it more likely that a person’s brain will also show Aβ aggregation? To rule out this possibility, the researchers looked for Aβ aggregation in 116 other patients who had died from sporadic or inherited (i.e. not infectious) prion diseases. These 116 patients had not acquired their prion disease from infected human growth hormone. They found that none of the patients in this control group had similar Aβ aggregation. They next asked whether Aβ aggregates could be found in the region of the brain where human growth hormone had been extracted from the cadavers. They examined the brains of an additional 49 patients who had died from Alzheimer’s, and indeed found Aβ aggregates in this particular brain region in 7 of these patients.
Based on their comprehensive findings (summarized in Figure 3), the researchers concluded that the extensive Aβ aggregates in these patients were likely triggered by small Aβ clumps contained in the cadaver-extracted human growth hormone. These cadaver Aβ clumps had very likely led to the misfolding and aggregation of normal Aβ protein in these patients’ brains. This finding represents the first observation of human-to-human Aβ transmission and perhaps the first indication that Alzheimer’s disease may be transmitted among humans in a similar fashion as prions.

So what does this study mean?
At this point, it is essential to immediately squash the growing fear that may now be slowly spreading in the back of your mind. These findings in no way imply that it is possible to contract Alzheimer’s disease through casual contact. What is implied is that extra precaution may need to be taken during surgery and invasive brain procedures, as is done with prion diseases, to ensure that tools are not contaminated with Aβ aggregates. This does not mean that one should avoid life-saving surgeries or blood transfusions due to fear of Alzheimer’s transmission. Transmission of prion diseases via medical procedures is extremely rare. In the past 4 decades, only 450 cases have been reported worldwide, half of which resulted from injection with PrP-contaminated human growth hormone [6]. Furthermore, previous population studies have found no correlation between Alzheimer’s disease incidence and a history of blood transfusion [6,9].
While this is a very compelling study, there are many limitations that need to be addressed. For one thing, this study only examined a very small sample of patients, and it is never a good idea to draw definitive conclusions based on a sample size of 8. Furthermore, this study only looked at one very specific mode of transmission: injection of cadaver-derived growth hormone. Other routes of transmission, if any, remain to be examined. Finally, as the authors themselves point out, these patients never developed clinical signs of Alzheimer’s disease, so it is impossible to say whether these observed Aβ pathologies would have actually resulted in clinical disease. What is important about this study, however, is that it provides additional human-based evidence to support the pile of test tube and animal model-based evidence suggesting that Aβ aggregates may behave similarly to prion aggregates, and that Alzheimer’s disease may indeed be more similar to prion diseases than we originally thought.
Danielle Heller is a PhD candidate at Harvard Medical School in the Department of Microbiology and Immunobiology
References
1. Alzheimer’s Disease. (2015, March 5). Retrieved October 8, 2015, from http://www.cdc.gov/aging/aginginfo/alzheimers.htm
2. Protein Structure. http:// lectures.molgen.mpg.de/ProteinStructure/Levels/ . Retrieved November 1, 2015.
3. Irvine, G et al. (2008). Protein Aggregation in the Brain: The Molecular Basis for Alzheimer’s and Parkinson’s Diseases. Molecular Medicine, 14(7-8), 451-464.
4. Goedert, M. (2015). Alzheimer“s and Parkinson”s diseases: The prion concept in relation to assembled Aβ , tau, and α-synuclein. Science (New York, N.Y.), 349(6248), 1255555–1255555. doi:10.1126/science.1255555
5. Jucker, M., & Walker, L. C. (2015). Self-propagation of pathogenic protein aggregates in neurodegenerative diseases. Nature, 501(7465), 45–51. doi:10.1038/nature12481
6. Jaunmuktane, Z., Mead, S., Ellis, M., Wadsworth, J. D. F., Nicoll, A. J., Kenny, J., et al. (2015). Evidence for human transmission of amyloid-β pathology and cerebral amyloid angiopathy. Nature, 525(7568), 247–250. doi:10.1038/
7. Christensen, J. (2015, September 10). No, Alzheimer’s is not contagious. CNN.com. Retrieved October 8, 2015, from http://www.cnn.com/2015/09/10/health/no-alzheimers-is-not-contagious/
8. Kunkle, F. (2015, September 9). Study: Alzheimer’s pathology might be transmissible via medical procedures. The Washington Post. Retrieved October 8, 2015, from https://www.washingtonpost.com/local/social-issues/study-alzheimers-could-be-transmitted-via-medical-procedures/2015/09/09/fcb22794-5648-11e5-8bb1-b488d231bba2_story.html
9. O’Meara, ES, et al. (1997). Alzheimer’s disease and history of blood transfusion by apolipoprotein-E genotype. Neuroepidemiology, 16(2), 86-93.

